Fistula Treatment
Laser treatment for fistula in ano- A sphincter saving approach
AETIOLOGY
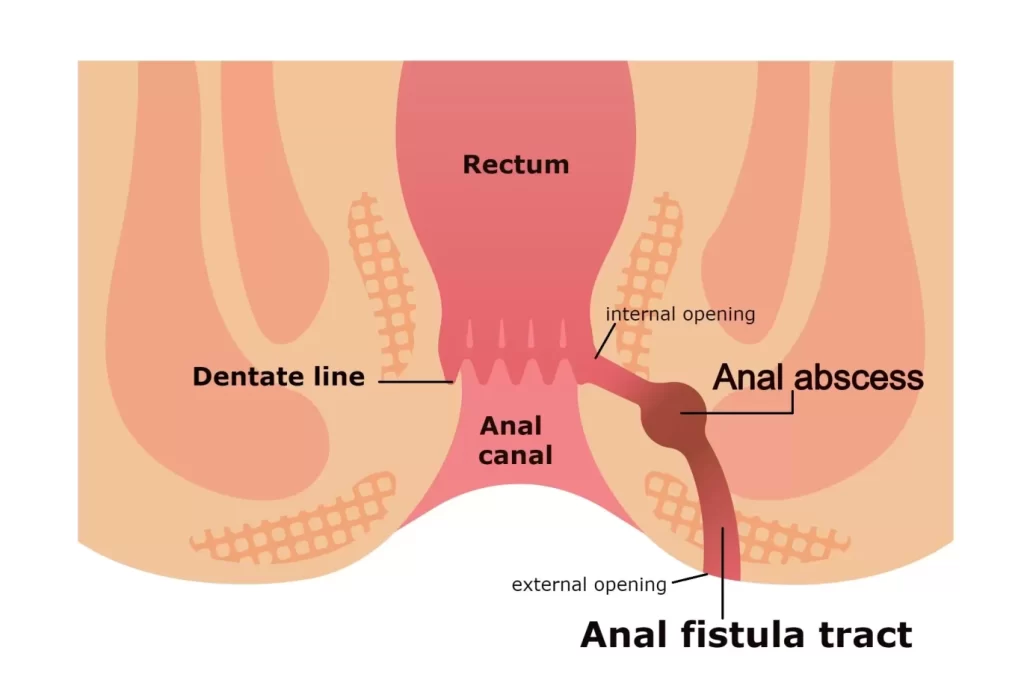
- Infection of the crytoglandular glands extending to the intersphincteric space leading to abscess formation which ultimately drains into the perineum leading to a track lined by granulation tissue and epithelial cells with an inner and outer opening.
- Secondery fistula- crohns, tb,lgv, trauma etc
FISTULA IN ANO
- DEFFINITION : A fistula-in-ano is an abnormal hollow tract or cavity that is lined with granulation tissue and that connect a primary opening inside the anal canal to a secondary opening in the perianal skin. Secondary tracts may be multiple and can extend from the same primary opening
- CRYPTOGLANDULAR FISTULA
- NON CRYPTOGLANDULAR FISTULA
AIM FOR THE IDEAL TREATMENT OF ANAL FISTULA
- Eradicate sepsis
- Promote healing of the tract
- Preserving sphincters and mechanism of continence
- Low rate of recurrence
METHODS FOR THE TREATMENT OF ANAL FISTULA
- Conventional laying open of the fistulous tract
- Seton
- Lift/bio-left
- Anal fistula plug
- Fibrin glue
- Video-assisted anal fistula treatment
- Laser fistula closure
- Adipose-derived stem cell
LASER IN THE MANAGEMENT OF FISTULA IN ANO
- Laser fistula closure (filac) method
- Distal laser with proximal ligation (dlpl) method
PROCEDURE FOR FILAC
- 1470nm/980 nm diode laser
- 600 micron radial laser emitting fiber(360 degree fiber)
- Laser energy is emitted from the up at 360 degree
- Energy causes shrinkage of the tissue and leading to the clouser of the tract.
- Fiber is slowly withdrawn at 1mm/sec
- 10w-12w energy per second is usually delivered
- Limited radial penetration depth (2-3mm beyond the fistula track)
WHETHER TO CLOSE THE INTERNAL OPENING?
- Non closure
- Mucosal advancement flap
- Anodermal flap
NON CLOSURE OF THE INTERNAL OPENING
- The FiLaC approach is designed to destroy both the crypt gland and the additional epithelial layer of the fistula track simultaneously by a photothermal effect with coincident obliteration of both the internal and external fistula orifices.
- RECURRENCE RATE : Higher
- EXPLANATION : The result of fistula re-opening with a linking up of the epithellal remnants of small undetected secondary tracks before the denaturaion effect of the laser can take effect.
DLPL-DISTAL LASER PROXIMAL LIGATION
- 1470nm /980nm DIODE LASER
- 600micron Radial Laser Emerging Fiber
- Identifying The Tract And Inner Opening By Gentle Probing Or Hydrogen Peroxide
- Dissecting The Tract In Between The External And Internal Sphincteric Plane
- Ligating The Tract Near The Mucosa And Cutting It.
- The rest of the tract was treated as per the Filac procedure.
CLOSURE OF THE INTERNAL OPENING
- Recurrence Rate : Less
- Preferred
- Complicated Fistula
LITERATURE REVIEW
- Primary Healing Rate 06.2%
- Secondary Healing Rate 05.5%
- Primary Healing Rate 71.4%
- Primary Healing Rate : 81.8%
COMPLICATIONS
- IMMEDIATE : BLEEDING
BURN - DELAYED : INCONTINENCE
FAILURE OF CLOSURE
ABSCESS FORMATION
COMPARING DLPL AND FILAC
DLPL
- For Complex Fistula
- Dissection Of The Intersphincteric Plane Required
- If Interspincteric Absess is Present It Gets Drained
- Recurrence Rate Is 5%
- No Sphincter Injury
DLPL
- For Straight Fistulous Tract
- No Such Dissection Required
- No Drainage
- Recurrence Rate Is 15%
- Quicker Post Op Recovery
- No Sphincter Injury
LASER AS AN IMPORTANT TOOL FOR PROCTOLOGIST
- LASERS provide newer treatment options.
- providing faster recovery.
- Lesser pain.
- Better outcome of surgery.
- Smaller wounds
- Making proctology a day care procedure
HAEMORRHOIDS
- World wide prevalence from 2.9% to 27.9%
- Men more the females
- Effects at middle age
- The anorectal vascular cushions along with the internal anal sphincter are essential in the maintainence of continence by providing soft tissue support and keeping the anal canal closed tightly.
- There are typically three major anal cushions , located in the right anterior, right posterior and left lateral aspect of the anal canal and various numbers of minor cushions lying between them
GRADATION OF HAEMORRHOIDS
Internal Hamerrhold Grades
No prolapse, just prominent blood vessels
Prolapse upon bearing down, but spontaneous reduction
Prolapse upon bearing down requiring manual reduction
Prolapse with inability to be manally reduced
About Seva Hospital
At Seva Hospital, we specialize in Piles, Maternity, and Surgical care, offering a range of treatments designed to ensure your health and well-being.
Quick Links
- Home
- About Us
- Our Services
- Gallery
- Blog
- Contact Us
Our Services
Copyright © 2024 Seva Hospital All rights reserved. | Design & Developed By Digital Gyan Technology